Diagnostic Technologies: Benefits And Risks
Today women are well aware of their 1 in 8 lifetime risk of breast cancer. Every year multiple awareness campaigns focus on identification of risk factors, yearly screening, early diagnosis, and subsequent treatment of breast cancer. Many women are subjected to yearly mammography screening in the hopes of early detection of breast cancer. However, after many years of its repeated use on thousands of women, the risks are being highlighted and new guidelines are being discussed. It is up to the individual woman and her physician to determine the usefulness of a routine mammogram, however many experts are now critical of yearly mammography for every woman over 40 years old.
A recent study1 published in the British Medical Journal reports that after a twenty-five year follow up of approximately 90,000 women there was no significant reduction in deaths from breast cancer with routine mammography. Twenty-two percent of breast cancers in the mammography group were unnecessarily diagnosed and over treated. This meant that these healthy women were subjected to repeated mammography, biopsies, subsequent surgeries, and other harsh treatment for breast cancer that was not dangerous.
In addition to breast cancers, routine mammograms, CT scans and other radiographic screening of cancers of the lung and thyroid are also among major controversial topics with unclear guidelines. These screening programs have failed to produce the expected results to reduce deaths from late stage cancers. On the other hand, there is a disproportionate increase in the diagnosis and treatment of early stage cancers or precancerous conditions, especially those in the breast, prostate and thyroid.
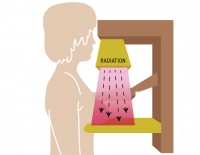
Several factors determine the usefulness of mammograms in an individual woman. A generic recommendation of a yearly mammogram for all women above the age of 40 has serious risks from repeated radiation exposure. The breast, thyroid, bone marrow, digestive, and reproductive organs are more sensitive to radiation damage because of continuous cellular growth activity in these tissues. Radiation exposure can vary by each mammogram, the machines used, and the person conducting the screening. Sometimes radiation from one mammogram can be equal to that received from 75 chest X-rays. We have summarized the hazards of radiation exposure from various screening technologies and the ways micronutrients can protect the body in a review article2. Micronutrients such as green tea extract, quercetin, resveratrol, and many others provide protection to the rapidly dividing cells, and protect the cellular structures like DNA, chromosomes, and mitochondria. Curcumin not only protects the radiation sensitive organ systems, but it also increases the activity of the genes responsible for cancer cell death. Vitamin C, E and N-Acetyl Cysteine protect cells even when taken immediately after radiation exposure.
Precancerous conditions such as ductal carcinoma in situ (DCIS) are increasingly diagnosed and treated as breast cancer because it can be detected only on mammography. DCIS is an accumulation of abnormal cells present only in the milk ducts without any palpable lump. This diagnosis was almost nonexistent before the routine mammography started. Now DCIS constitutes 20% of all breast cancers.
An open discussion with their physician is the key to determine every woman’s requirement to get a mammogram while minimizing the health risks of such radio-diagnostic tests. In addition, it is very important to ensure an optimum daily intake of antioxidant nutrients and increase it as necessary.
Ref:
- Miller AB, et al., BMJ. 2014 Feb 11;348:g366.
- How to use diagnostic technologies wisely and for the benefit of your health