 Dr. Rath Cellular Health™
Dr. Rath Cellular Health™
Worldwide, more than 100 million people suffer from diabetes, characterized by a high sugar level in the blood. The reason for it is either insufficient insulin production, the hormone responsible for sugar metabolism, or impaired cellular response to this hormone.
Diabetic disorders have a genetic background and are divided into two types: juvenile or Type I and adult, also called Type II diabetes. Type I diabetes is generally caused by a genetic defect that leads to an insufficient production of insulin in the pancreas and it requires regular insulin injections to control blood sugar levels. The majority of diabetic patients, however, develop this disease as adults. Adult or Type II forms of diabetes also have a genetic background. However, the causes that trigger the outbreak of the disease in these patients at any stage in their adult lives have been unknown. It is, therefore, not surprising that diabetes is yet another disease that is still growing on a global scale.
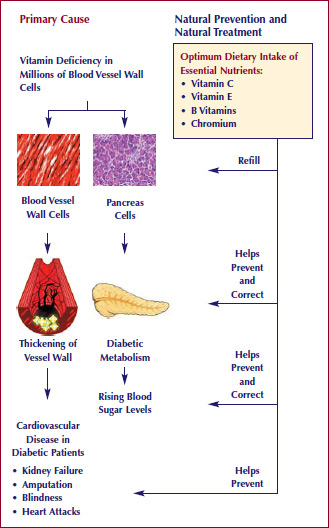
Cellular Medicine now provides a breakthrough in our understanding of the causes, prevention and adjunct treatment of adult diabetes. The primary cause of adult onset diabetes is a long-term deficiency of certain vitamins and other essential nutrients in the millions of cells in the pancreas (the organ that produces insulin), the liver and the blood vessel walls, as well as other organs. In individuals with inherited diabetic predisposition, deficiencies of vitamins and other essential nutrients can trigger a diabetic metabolism and the onset of adult diabetes. Conversely, the optimum intake of vitamins and other essential nutrients can help prevent the onset of this disease and help correct existing diabetic conditions and its complications.
The key to understanding cardiovascular disease in diabetics is to recognize the similarity in the molecular structure of vitamin C and sugar (glucose) molecules. This similarity can lead to metabolic confusion in the process to transporting glucose and vitamin C molecules through cellular membranes. With an abundance of glucose in the bloodstream, the transport of vitamin C molecules through cellular membranes of vascular cells becomes blocked resulting in vitamin C deficiency conditions inside these cells. For the cardiovascular system vitamin C deficiency has especially severe consequences as it leads to developing cardiovascular deposits not only in the arteries of the heart, but also in blood vessels in the legs, eyes and other organs in the body.
Therefore, the decisive measure for preventing cardiovascular complications in diabetes is by the optimum daily intake of selected cellular nutrients – in particular vitamin C. Clinical data have shown that with high intake of vitamin C the requirements for insulin becomes lower.
The results of a pilot clinical trial have shown that the optimum intake of a combination of vitamin C with other vitamins, amino acids and minerals, such as chromium, has resulted in lowering of glucose levels in the blood and a decreased glycosylated hemoglobin index (an indicator of the damage to red blood cells caused by sugar). Nutrients acting in a synergy help to restore the balance between vitamin C and sugar metabolism inside the cells of the pancreas, blood vessel walls and other organs, which is compromised in a diabetic state.