Micronutrient Synergy May Prevent Antimicrobial Resistance
Globally, resistance to treatment with antimicrobial drugs is becoming an increasingly serious public health problem. Antimicrobial resistance is a larger phenomenon than antibiotic resistance. In addition to drug resistant bacteria, the antimicrobial resistant species also include other drug resistant microbes such as fungi, parasites, and viruses. According to the World Health Organization (WHO), 480,000 new cases of multi drug resistant tuberculosis (XDR-TB) were diagnosed in 2013. Other disease causing and highly virulent organisms that have already developed drug resistance are malarial parasites, the fungus Candida, methicillin-resistant-Staphylococcus aureus (MRSA), and the bacteria causing gonorrhea. The drug resistant bacteria are estimated to cause 99,000 deaths in U.S. hospitals every year.
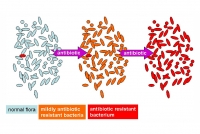
Factors such as frequent and unnecessary use of antibiotics in patients with viral infections, not completing the prescribed course of antibiotics treatment for bacterial infections, and an abundant use of antibiotics in animal feed contributes to the development and spread of drug resistant microbes. Even, simple preventive measures such as hand washing are not commonly used. This is critical especially in hospital settings where drug resistant bacteria are extensively present. Hospital acquired infections is one of the fastest way of spreading the drug resistant bacteria and other microorganisms within the communities. Patients with infections caused by drug-resistant bacteria are generally at increased risk of complications and death, more so than patients infected with the same bacteria that are not resistant. According to the Centers for Disease Control (CDC), every year an estimated 648,000 people in the U.S. develop infections during their hospital stay. In a recently published study in the British Medical Journal, the authors concluded that the most commonly used antibiotics could soon be ineffective, especially in children with urinary tract infections (UTI), and respiratory, and other infections, because the children continue to carry and spread these resistant bacteria for more than six months after the treatment. Therefore, search for methods to control this problem is urgently required.
Our researchers conducted a study using the drug resistant bacteria responsible for the most common infections. Specific strains of bacteria, such as Staphylococcus (UTI, respiratory, skin infections), E. Coli and Salmonella (food poisoning, UTI, anemia, kidney failure and death), and L. monocytogens (flu like symptoms), were used in the study*. These bacterial strains used in this study were highly resistant to the commonly used antibiotics. When subjected to a specific micronutrient combination containing vitamin C, lysine, proline, and green tea extract, these drug resistant strains of bacteria showed increased susceptibility to the antibiotics. We also studied the similar effects on the bacteria by using vitamin C alone. Although vitamin C helps increase the antibiotic susceptibility of the bacteria, our results indicate that, the combination of antioxidant micronutrients has a significantly higher effect than vitamin C alone.
Irresponsible use of antibiotics is contributing to the development of drug resistant bacteria; and is threatening our world with a situation similar to before the discovery of penicillin when there was no effective treatment for infections. Our study gives hope that use of specific micronutrients can help and increase the vulnerability of these organisms to current antimicrobial treatments.
*Harakeh S. et al., African J of Microbial Disease, Vol. 7(20), pp. 2351-2358, 2013