Why Cholesterol Is Not the Cause of Heart Disease
Dr. Rath’s discovery of the vitamin C-scurvy-heart disease connection and our latest research shed new light on the role of cholesterol in heart disease.
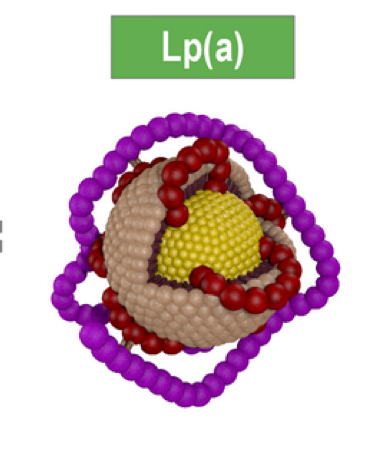
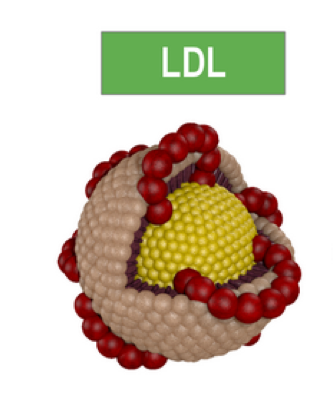 LpaLDLHigh blood cholesterol can lead to cardiovascular deposits only when combined with the loss of the integrity and functional weakness of the blood vessel walls. Weakened arterial wall structure triggers the need for its biological repair. The most common cause of vascular wall dysfunction and an increase in vascular endothelial gaps allowing for infiltration of large biological molecules (Lp(a) and LDL) is a long-term deficiency of vitamin C and other micronutrients (vitamin B6, Copper, Lysine, etc.). These micronutrient deficiencies can lead to insufficient production or impaired structure of collagen, the protein which forms the basic structure of blood vessels. Such structural weakness is first manifested in the blood vessel wall areas exposed to highest mechanical stress, such as the coronary arteries. In this situation, vascular deposition of blood lipoproteins, in particular Lipoprotein(a), works like a biological “plaster” reinforcing factor.
LpaLDLHigh blood cholesterol can lead to cardiovascular deposits only when combined with the loss of the integrity and functional weakness of the blood vessel walls. Weakened arterial wall structure triggers the need for its biological repair. The most common cause of vascular wall dysfunction and an increase in vascular endothelial gaps allowing for infiltration of large biological molecules (Lp(a) and LDL) is a long-term deficiency of vitamin C and other micronutrients (vitamin B6, Copper, Lysine, etc.). These micronutrient deficiencies can lead to insufficient production or impaired structure of collagen, the protein which forms the basic structure of blood vessels. Such structural weakness is first manifested in the blood vessel wall areas exposed to highest mechanical stress, such as the coronary arteries. In this situation, vascular deposition of blood lipoproteins, in particular Lipoprotein(a), works like a biological “plaster” reinforcing factor.
According to this new understanding, high blood cholesterol is a “consequence” of, not the “cause” of, heart disease.
This concept also answers why heart attacks are the leading cause of death in humans, but are an exception in the animal world. All animals, with only a few exceptions, produce large quantities of vitamin C in their bodies (2-20 grams/day) to support optimum collagen production necessary for maintaining healthy and elastic blood vessels. A high level of endogenous vitamin C production protects animal arteries from damage and development of atherosclerotic deposits. This is why animals do not die of heart attacks, even if some, such as bears, have very high blood cholesterol levels (600 mg/dl). In contrast, humans lost the ability of vitamin C production, and its daily dietary intake is often insufficient to assure optimum vascular health. For humans, the recommended dietary allowance (RDA) for vitamin C is 60-80 mg/day.
 A summary of Dr. Rath’s groundbreaking discovery is outlined in a PDF Cholesteral discovery, and it is also presented in his popular book Why Animals Don’t Get Heart Attacks, But People Do!
A summary of Dr. Rath’s groundbreaking discovery is outlined in a PDF Cholesteral discovery, and it is also presented in his popular book Why Animals Don’t Get Heart Attacks, But People Do!
Cardiovascular Research at the Dr. Rath Research Institute
Our research in the area of cardiovascular disease focuses on the health-beneficial effects of vitamins and essential nutrients in various aspects of cardiovascular disease, its initiation, and stepwise progression.
Our researchers developed a new mouse model (GULO-/-;Lp(a)+) which has two characteristics of human metabolism: the expression of Lipoprotein(a) and the lack of endogenous vitamin C (ascorbate) production. We showed that dietary deficiency of vitamin C resulted in increased serum levels of Lp(a). Moreover, chronic suboptimal intake of vitamin C and its complete depletion (scurvy) leads to Lp(a) accumulation in the vascular wall and parallels atherosclerotic lesion development. Our results confirm that dietary vitamin C deficiency is a risk factor for atherosclerosis independent of dietary lipids. Our scientific work supports the concept that Lp(a) functions as a mobile repair molecule compensating for the structural impairment of the vascular wall, a morphological hallmark of hypoascorbemia and scurvy.
Among other projects, we have been investigating the role of nutrients in controlling abnormal migration and the growth of smooth muscle cells in the arterial wall, a hallmark of atheroma development and growth. We are also studying how nutrient synergy can be applied to curb inflammation leading to arterial wall cell damage and blood leukocyte recruitment. We have shown that nutrient synergy is more effective than individual antioxidants in decreasing oxidative stress associated with endothelial and smooth muscle cell damage, and lipid and lipoprotein oxidation and their intra-arterial wall accumulation.
A significant part of our efforts have been concentrated on applying nutrient synergy in controlling pathological aspects of the remodeling of the extracellular matrix in the arterial wall. Such pathology leads to lost integrity and weakening of arterial wall structure, impaired arterial contractility, lipoprotein retention and oxidation, pathological behavior of arterial wall resident cells, increased plaque instability and the risk of its rupture.
Our other research areas include the aspects of sex hormone imbalance in the development of cardiovascular disease, as well as the cardiovascular aspects of impaired glucose metabolism (diabetes mellitus). Our research findings have contributed to a better understanding of nutrient synergy in controlling uterine smooth muscle tissue contractility (important in preventing miscarriage) and in autoimmune mechanism-mediated impairment of bronchial smooth muscle tissue contractility (asthma).
Studies in Heart Disease